Using AI to control energy for indoor agriculture
30 September 2024
Published online 7 July 2011

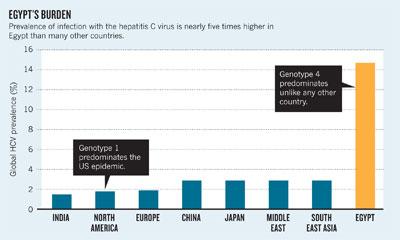
Egypt is a hepatitis C anomaly. Globally, roughly 1 person in 50 is infected with the hepatitis C virus (HCV). In Egypt, a recent study found that about one person in seven of Egypt's 83 million population tested positive for antibodies against HCV, indicating that these individuals have been infected with the virus at some point. However, nearly one person in ten carries its viral RNA and is therefore chronically infected.
This represents a huge viral reservoir that is fuelling the spread of the disease among Egyptians, mainly through hospitals and clinics (medical and dental; private and public). Firm data for the infection rate are hard to come by. A 2010 study estimated that more than half a million people are newly infected each year. However, the Egyptian Ministry of Health and Population (MOHP) puts the number at 100,000 per year. Both numbers should be much lower, says Laith Abu-Raddad, an epidemiologist at the Doha-based Weill Cornell Medical College in Qatar and co-author of the 2010 study. He questions why there are so many new cases of a preventable infection each year.
Not only is the Egyptian HCV problem one of size, but the genotype of the virus in circulation is one that is not commonly found in the rest of the world. If it is not controlled, there's no guarantee that it will be confined to Egypt. Cheaper travel and increased migration means that Egypt's HCV problem is already starting to spread to Europe and the rest of the world.
Egypt's current problem with hepatitis C arose after an earlier — successful — health campaign against a different type of pathogen. Schistosomiasis is a disease caused by a parasitic worm that can burrow through skin and lurks in contaminated water. The worm then travels to the lungs and liver, where it matures and moves to other organs. During the early part of the twentieth century, schistosomiasis was highly prevalent in Egypt, especially in rural areas, and was a major cause of liver disease. From the 1950s to the early 1980s, the MOHP and the World Health Organization (WHO) led a large-scale campaign to control the disease. Millions of people were treated with intravenous injections of tartar emetic, before an oral drug replaced this standard of care across the country in the 1980s.
Although the campaign helped reduce the prevalence of schistosomiasis, this came at a price. At the time, little was known about hepatitis or about the causative viruses and their transmission. Reuse of glass syringes and lax sterilization practices caused widespread infection with HCV, which by the 1990s had replaced schistosomiasis as the primary cause of liver disease in Egypt.
The virus that was spread by this programme has a different genotype from HCV in most other countries. Egypt — and the Middle East more generally — is a stronghold for genotype 4. By contrast, about 75% of HCV infections in Europe and the United States are of genotype 1. Consequently, most research conducted in the West has gone into the control and treatment of that genotype; there have been comparatively few studies on how to improve the treatment of patients with genotype 4.
The dominance of genotype 4 in Egypt complicates the task of treating the disease. "There are no antiviral drugs being developed locally to combat genotype 4," says Alaa Ismail, head of the liver research unit at Ain Shams University in Cairo. The treatments available to people with hepatitis C in Egypt are therefore imported from the West and have been extensively tested only on genotype 1. "All the drugs that we get from overseas must undergo clinical trials here again," he says.
The best estimate for genotype 4 is that only 60% of those treated clear the virus completely. Although this is better than the cure rate for genotype 1 (at about 50%), it is still inadequate and new treatments are needed. But most Egyptians struggle to afford even the existing drugs. A full, 48-week course of HCV medication costs around US$3,500 — well above the Egyptian median income of US$2,070 per person each year.
The MOHP has two programmes in place to tackle HCV infection — one targeted at treating chronic, symptomatic patients, and one aimed at prevention.
Through the treatment programme, the MOHP provides free or subsidized treatment for the millions of infected people who cannot afford the drugs. It is one of the largest burdens on the healthcare system in Egypt. Yet despite the large number of patients and the high cost of the treatment regimen, the MOHP argues that it is more cost effective than treating patients after they develop serious complications such as liver cirrhosis or liver cancer.
DeWolfe Miller, an epidemiologist at the University of Hawaii in Honolulu and one of the first to discover the Egyptian epidemic, in 1992, says: "There are national centres for HCV treatment, but there has been criticism regarding access and the quality of drugs used. I estimate that these programmes reach approximately 30% of the total number of Egyptians who are in need of treatment." Miller contends that diverting some of the MOHP's resources from treatment to prevention would be a better use of funds. "What is frequently misunderstood is that treatment, however important that may be, does not reduce or prevent transmission," he says.
This is a socioeconomic disease, and while 60% of infections happen in hospitals and clinics, the rest are down to bad social practices.
At the core of the MOHP's prevention programme are public awareness campaigns, mainly run through television programmes and posters in hospitals, which have been in place for about ten years. According to Ismail, who was also director of the ministry responsible for the hepatitis C programmes — the National Hepatology and Tropical Medicine Institute (NHTMI) in Cairo — until 2006, the national centres for HCV have seen a decrease in the number of new infections over the past few years. This drop "can only be attributed to the awareness campaigns," Ismail says. "This is a socioeconomic disease, and while 60% of infections happen in hospitals and clinics, the rest are down to bad social practices, such as the sharing of razors at barber shops or the sharing of home diabetes testing equipment."
Miller, however, challenges the effectiveness of the prevention efforts. He points out that the virus continues to spread in Egypt. "It is the responsibility of all healthcare professionals to provide safe healthcare." Indeed, he says, health-care professionals could take a big step towards slowing the spread of HCV in Egypt by simply maintaining clean facilities. "The HCV is so fragile that it can be disinfected with soap and water."
The MOHP is taking action on this front. In 2008, it began a new campaign, with two major elements. "The first is education, where we regularly teach hospital staff about infection control," says Mohamed Ezz El-Arab, head of the tumour unit at NHTMI. "Second, every hospital now must have an infection control committee which has clear authority to monitor what is going on in the hospital."
Furthermore, HCV and infection control is now an important course that is taught in all medical universities, unlike the brief mention it received a few decades ago. There are also meant to be regular inspections of public hospitals and clinics to ensure that they meet the infection control standards set by the WHO and that proper waste-disposal protocols are in place.
Critics like Miller say that actions speak louder than words. He remains unconvinced of the programme's value or of its implementation. There have been recorded instances, he says, where public hospitals have dumped their waste "directly, without treatment, into the solid waste stream", violating WHO specifications. "This is a scandal."
Just last October, the Egyptian weekly magazine Rose al-Yousef reported that dialysis filters had been found in the non-medical waste disposal in front of a university hospital. Rubbish scavengers had been washing and reselling them for a fraction of their original price. In 2008, the Egyptian daily Al-Masry Al-Youm reported that truckloads of medical waste, including blood bags, had been delivered to garbage collectors for reuse.
Disposing of medical waste in this way is highly unsafe and risks passing on the virus. Medical waste disposal is "better controlled in Cairo now," says Ezz El-Arab. "But while we can follow-up on what is happening in Cairo, the problem is in rural areas further away where monitoring is hard."
Measuring the success of these HCV programmes is hard because there are no objective data available. "Only those in the MOHP have any information on the status of this programme," Miller says. Without good data, it is not possible to verify whether the rate of new HCV infection in Egypt is decreasing. And even if there has been a drop in the rate, the overall level of infection is still much higher than anywhere else in the world. It can take 20 to 30 years of HCV infection before people develop serious complications. So the worst effects of the epidemic will surface over the next few years.
There is a ray of hope. The MOHP is part of the government established by the former President Hosni Mubarak. Miller suggests that, after the popular revolution in early 2011 that toppled Mubarak, there may be an opportunity for implementing better prevention programmes as many of the ministries undergo changes. "Post revolution means that HCV prevention should and can be accomplished by non-governmental, non-profit organizations," he says. "The MOHP has to come clean with its failure to prevent or reduce HCV transmission." At the same time as creating a new government, perhaps the revolution will also offer a uniquely Egyptian solution to the HCV epidemic.
doi:10.1038/nmiddleeast.2011.83
Stay connected: