Using AI to control energy for indoor agriculture
30 September 2024
Published online 7 March 2012
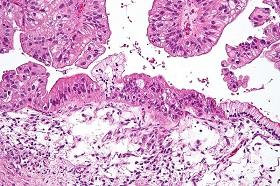
By the time most women with ovarian cancer are diagnosed, the cancer has spread to other parts of the body. These secondary lesions are usually more dangerous than the original tumour and make ovarian cancer one of the deadliest cancers.
Researchers have for the first time compared the characteristics of secondary lesions with the primary ovarian tumours by collecting biopsy samples from nine patients.
They found vast differences between the mutations of the original tumour and those of the secondary lesions. They publish their findings in the journal PLoS ONE.
"Some of the lesions are very similar to the primary tumour and some are very different you'd think they may have occurred before the primary tumour itself," says Arash Rafii, a geneticist at Weill Cornell Medical College in Qatar (WCMC-Q) who led the research. "A lot of the metastatic lesions do not have the same genes at all as the primary tumour."
Ovarian cancer has the worst survival rate of any gynecological cancer owing to its metastatic lesions. While chemotherapy and surgical removal of the primary tumour can be effective, the extensive spread of cancer throughout the abdomen leaves a poor survival rate of 20–30% of patients at five years.
Rafii began the study five years ago in France and did some of the work with the Agency for Science, Technology and Research (A *STAR) in Singapore. When he moved to QCMC-Q in Doha his team decided to finish the study there.
"By studying patients whose primary ovarian cancer is very similar, we have shown that the metastasized lesions, often the most dangerous part of the disease, are different. This means they may respond differently, possibly better, to a different cancer drug," explained Rafii in a press release.
Rafii suggests these findings might mean clinicians need to rethink their approach to treating ovarian cancer — which traditionally focuses on the primary cancer. "Instead of focusing on the primary tumour you need to look at the metastatic lesions as well for personalized treatment."
According to the authors, understanding the biology of the metastatic lesions is critical to the design of new therapeutic approaches.
"At this point we have characterised the copy number variation and not the mutation," says Rafii. His team is now looking at the actual mutations for further research.
While the genetic changes evident in the metastatic lesions are different, Rafii expects there is probably some pattern to the data waiting to be identified. "We received a lot of samples after the study was published from Montreal and France. So now we are asking if we can cluster the patients by the biology of the metastatic lesions, or at least by the differences between the primary tumour and the metastatic lesions.
"We are looking for the common core which we can target — what is really always there for all patients, and then go deeper into how we can treat a single patient."
doi:10.1038/nmiddleeast.2012.29
Stay connected: