Using AI to control energy for indoor agriculture
30 September 2024
Published online 11 March 2015
Qatari researchers have found that ovarian cancer cells communicate with blood vessels to resist a commonly used anti-cancer drug.
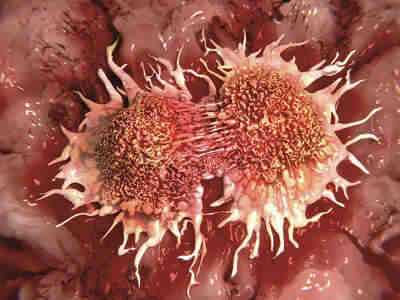
Ovarian cancer is the seventh most prevalent cancer in women worldwide and the 5th most common cancer among women over 15 in Gulf states. It causes tens of thousands of deaths annually and statistics show that just 45% of women with ovarian cancer are likely to survive five years from diagnosis.
WCMC-Q scientists looked at ovarian tumour microenvironments to learn how they “communicate” with the inner lining cells of blood vessels, known as vascular endothelial cells.
“We show a role for the endothelium to sustain tumours regardless of tumour perfusion,” says Arash Rafii, associate professor of genetic medicine at WCMC-Q, about the study published in Molecular Cancer Therapeutics.
“We think that we have the drugs that can efficiently kill cancer cells. However, the solution lies in better understanding the interaction between cancer cells and endothelial cells and being able to design therapies that can disrupt the pro-tumoural niche [microenvironment].”
Bevacizumab is an anti-cancer drug that inhibits new blood vessel growth in a tumour by preventing vascular endothelial growth factor (VEGF) from binding to its receptor. This ultimately cuts off the tumour’s nutrient and oxygen supply and blocks off entry points for metastases to enter the circulation.
But despite an initial positive effect, withdrawing the drug can result in rapid tumour regrowth with accelerated decline in patients’ wellbeing. Most tumours develop resistance to bevacizumab over the long term.
By studying ovarian cancer cell lines in culture, WCMC-Q researchers found that communication between cancer cells and vascular endothelial cells results in the activation of a pathway, called the Akt pathway, which causes endothelial cell proliferation. This stimulates new blood vessel growth.
While their research showed that bevacizumab did neutralize VEGF in ovarian cancer cells, the team detected levels of a growth factor known as fibroblast growth factor (FGF). This stimulates the synthesis of fibroblasts, the most common cell in connective tissue. FGF levels are reported to be elevated in ovarian cancer patients.
They found that blocking FGF had a minor effect on the movement of newly forming blood vessels, but it drastically impaired the formation of vascular tubes. This seems to point to the role of FGF as a potent factor involved in blood vessel formation.
The researchers also found that FGF was able to induce Akt-activation in endothelial cells, even when VEGF was inhibited. Treating endothelial cells with FGF led to bevacizumab resistance.
The team neutralized FGF with an antibody, which led to a decrease in the normal function of the Akt pathway in endothelial cells. When bevacizumab was added to anti-FGF, there was a synergistic effect. This suggests that Akt activation of endothelial cells depends on the secretion of both VEGF and FGF.
Blocking FGF alone did not impact the survival of the endothelial cells. However, it did reverse resistance to bevacizumab.
It seems that in tumours, the endothelial cells not only induce blood vessel formation, but they also transform into a host cell able to sustain tumour growth, explains Rafii.
The researchers believe that the FGF and Akt pathways could be a target for therapeutic strategies in cases of ovarian cancer that are resistant to bevacizumab.
“It seems that FGF secreted by the tumour cells could act as a proangiogenic cytokine. It is yet hard to know whether FGF is the only responsible [factor],” he adds.
The study sheds further light on the mechanisms involved in clinical resistance to anti-VEGF therapies. “We are moving toward a better understanding … but we still do not have a verified solution,” says Rafii. “These studies open more of an avenue for further exploration than bringing a cure,” he emphasises.
doi:10.1038/nmiddleeast.2015.46
Stay connected: