Using AI to control energy for indoor agriculture
30 September 2024
Published online 7 December 2020
New HIV infections have risen sharply in the past decade across the Middle East and North Africa, despite falling numbers at the global level.
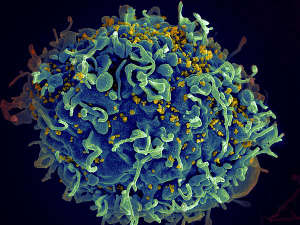
Seth Pincus, Elizabeth Fischer and Austin Athman, NIAID/NIH
The report identifies several factors behind this rise.
Humanitarian crises across several Arab states are a considerable challenge for HIV/AIDS programmes. Constraints on civil society organizations are also a major hurdle, since they are often the first line of defence against the virus.
“Current HIV programmes often fail to reach the people that are most at risk of acquiring the infection, as these populations tend to be hidden and stigmatized,” explains Hiam Chemaitelly, a senior epidemiologist at Weill Cornell Medicine College in Qatar (WCMC-Q).
UNAIDS executive director Winnie Byanyima says that progress is being made in testing and treatment, but there is less progress in prevention. She points out that several demographics are witnessing rising infection rates in MENA, Eastern Europe, Central Asia and Latin America.
According to the UNAIDS report, 43% of new infections are occurring among people injecting drugs, 31% are sex workers and their clients, and 23% are through sexual intercourse between men. All three are criminalized in most MENA states. They are often also vilified by society, with around 80% of people aged 15 to 49 saying they would not buy vegetables from a shopkeeper living with HIV. Byanyima stresses that more work is needed, not only to reform laws, but to address social norms and people's attitudes and beliefs.
In 2019, Chemaitelly and her colleagues published a study documenting the rapid rise in HIV infections among female sex workers and their clients. On average, only 18% of female sex workers in the MENA region ever tested for HIV, and even fewer tested for HIV in the past 12 months. “This is far below the 90% service coverage target set by UNAIDS,” she says.
The region’s research efforts
Several HIV research projects are being conducted in the MENA region to understand epidemiological, behavioural, and clinical aspects of HIV. However, compared to other regions, efforts are too limited to yield substantial and useful data.
Some areas of HIV research, such as studying the virus itself and developing new treatments, are challenging to conduct due to the substantial resources required. However, other types of HIV research, such as epidemiology studies, can be expanded, as the region has the necessary human capital and they require fewer resources. This type of research is crucial for informing the development of effective strategies, expanding current programmes and ensuring proper monitoring of the epidemic.
The real challenge facing researchers in this field is securing funding for their projects. A decade ago, the increase in funding was instrumental in HIV research expansion and allowed the detection of several nascent or established epidemics in the region. But Chemaitelly is concerned about the continuous decline in funding in recent years. “I am worried that the progress achieved over the last decade will be undermined at a time when the HIV epidemic continues to expand in this region.”
Human rights to win the battle
HIV treatment is generally available and typically provided free of charge, but HIV testing rates are low among populations most at risk. Most of these populations remain unaware of their HIV status, and therefore do not access available treatments and may unknowingly pass the virus on to others.
Byanyima argues that the solution is not only in the biomedical field. “We have to work on the human rights barriers.”
“If we do not win in this area, no medical tool can help us win the battles that remain,” says Byanyima.
doi:10.1038/nmiddleeast.2020.129
Stay connected: