Using AI to control energy for indoor agriculture
30 September 2024
Published online 28 February 2020
The molecular underpinnings of a severe immunodeficiency point researchers towards a more effective treatment.
Luigi D. Notarangelo
Enlarge image
The international study, which included researchers from several Saudi universities, analyzed data from six unrelated patients with a form of severe combined immunodeficiency, a group of genetic disorders in which patients lack white blood cells called T cells. Four patients had received stem cell transplants that had not led to T cell recovery.
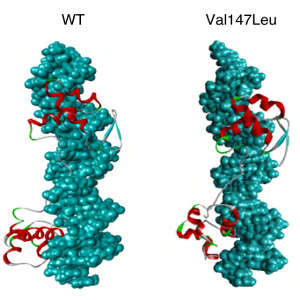
Sequencing revealed that all six patients had mutations in the PAX1 gene, which reduced the activation of the developmental genes it controls.
Stem cells from the patients were induced to differentiate into thymic progenitor cells. These had altered expression for genes involved in the development of the T-cell-producing thymus, revealing why stem cell transplants do not correct the immunodeficiency.
“We were surprised to see that PAX1 deficiency appears to have a more critical role in humans than in mouse models,” says Luigi Notarangelo of the US National Institutes of Health. The thymic and skeletal defects are less severe in mice, while the T cell immunodeficiency is more severe in human patients. “This is yet another example of how we need to study patients and to model human diseases with human samples.”
The researchers recommend that PAX1 deficiency should be added to the list of severe T cell immunodeficiencies, and that PAX1 patients should receive a thymus transplant.
doi:10.1038/nmiddleeast.2020.29
Yamazaki, Y. et al. PAX1 is essential for development and function of the human thymus. Sci. Immunol. 5, eaax1036 (2020).
Stay connected: