Using AI to control energy for indoor agriculture
30 September 2024
Published online 18 May 2020
Parkinson’s disease is typically associated with large clumps of the protein α-synuclein, but primate studies suggest even tiny aggregates can set this disease in motion.
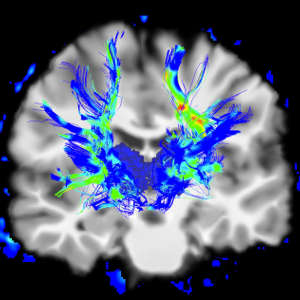
Image Source / Alamy Stock Photo
Parkinson’s patients typically exhibit accumulation of the protein α-synuclein within a brain region called the substantia nigra. These deposits, known as Lewy bodies, are associated with the death of neurons that respond to the neurotransmitter dopamine, leading to loss of motor function and, eventually, death.
Bezard and Dehay had previously shown that injections of patient-derived brain tissue containing Lewy bodies can trigger a chain reaction of Parkinsonian disease in mice and non-human primates. For this latest study, they assembled an international team of collaborators, including Omar El-Agnaf of the Qatar Biomedical Research Institute, to characterize how this pathology plays out in the baboon brain.
The results proved startling. “Our control injection, a sample not containing Lewy bodies, was also leading to the same extent of neurodegeneration,” says Bezard. These samples were also collected from Parkinson’s patients, but lacked detectable aggregates and were thought to primarily contain the soluble, non-pathogenic form of α-synuclein. Such ‘non-Lewy body’ injections do not cause disease in mice, but were clearly having a different effect in primates. Careful analysis revealed that this non-Lewy body sample contained a small fraction of tiny aggregates. These small clusters represented less than 10% of total α-synuclein, but were nevertheless able to cause serious neurological damage.
Bezard believes these findings could have important implications for how drug developers go about treating this disorder. “Most companies are trying to develop antibodies,” he says. “If they focus on targeting the big aggregates, they will miss these small aggregates that are as active in inducing pathology.” These results also suggest that Parkinson’s models focused on mice injected with Lewy bodies may not adequately capture key aspects of human disease pathology.
As part of this study, the researchers also used machine learning to study the pathology observed in baboons receiving these distinct injections, and the results suggested that disease triggered by non-Lewy body injections exhibits distinct features from Lewy body-induced disease. Bezard and colleagues are continuing to probe these differences in ongoing research, and to explore potential parallels and differences relative to other neurodegenerative disorders.
doi:10.1038/nmiddleeast.2020.56
Bourdenx, M. et al. Identification of distinct pathological signatures induced by patient-derived α-synuclein structures in nonhuman primates. Sci. Adv. 6, eaaz9165 (2020).
Stay connected: