Using AI to control energy for indoor agriculture
30 September 2024
Published online 20 January 2020
Newly identified gene mutation helps explain conditions linked to lung infections.
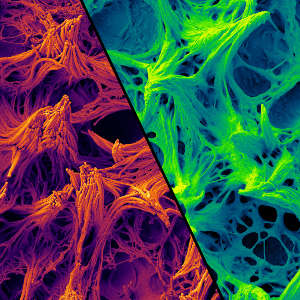
Raghu Chivukula and Koch Institute Nanomaterials Core Facility
Researchers found the gene NEK10 helps regulate the length and function of motile cilia, tiny hair-like structures that clear material from the airways in a process called mucociliary clearance. Mutated forms of NEK10 were identified in a group of patients with bronchiectasis, a condition that increases susceptibility to lung infections due to mucous build-up in abnormally wide airways.
Pulmonologist Raghu Chivukula of Massachusetts General Hospital in Boston, US sequenced the genomes of a female patient with bronchiectasis, and her two siblings who had similar symptoms. He found they shared NEK10 mutations.
Chivukula and colleagues observed that mutated NEK10 in cultured epithelial cells from the patient was still able to make its protein product, but only in an unstable form.
The researchers, including Fowzan S. Alkuraya of the King Faisal Specialist Hospital and Research Center, Saudi Arabia, then identified six other patients with bronchiectasis and NEK10 mutations. The team used the CRISPR-Cas9 genome-editing technique to remove NEK10 from healthy cells and found that cilia devoid of the gene moved abnormally.
“In the absence of NEK10, the cilia beat ineffectively because they were too short,” says Chivukula.
The discovery should help in the diagnosis of other patients with currently unexplained bronchiectasis, and may have wider implications. “This could lead to new insights and treatments, not just for bronchiectasis but more broadly, because mucociliary dysfunction is a feature or driver of other respiratory diseases, such as chronic obstructive pulmonary disease, asthma, and idiopathic pulmonary fibrosis,” says Louise Wain, British Lung Foundation Chair in Respiratory Research at the University of Leicester, UK. She was not involved in the research.
Previous research has revealed that cilia shortening could lead to breathing problems seen in smokers. Chivukula speculates that NEK10, which has not previously been linked to poor health in humans, could become a target for new treatments for smoking-related and other respiratory diseases.
“This raises the possibility that, perhaps with gene therapy or drugs, we might be able to augment NEK10 activity to make cilia work better in patients with conditions like chronic obstructive pulmonary disease and emphysema.”
doi:10.1038/nmiddleeast.2020.8
Chivukula, R. et al. A human ciliopathy reveals essential functions for NEK10 in airway mucociliary clearance. Nat. Med. https://doi.org/10.1038/s41591-019-0730-x (2020).
Stay connected: