Using AI to control energy for indoor agriculture
30 September 2024
Published online 28 May 2021
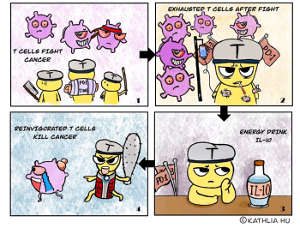
A new treatment promises to help immune cells recover from the ordeal of fighting off cancer.
Kathlia Hu
Enlarge image
Cancer immunotherapy involves stimulating the immune system to enhance its response against tumours. However, continued stimulation eventually exhausts T cells, making them unable to control tumour progression. Now, an international collaboration, which included a researcher at New York University Abu Dhabi, has shown that interleukin-10 (IL-10) treatment can reinvigorate a subset of these T cells, known as terminally exhausted T cells.
The team engineered a version of IL-10 with an extended half-life (IL-10-Fc), meaning it would persist longer in the body, and tested its effect together with adoptive T cell transfer (ACT) in mice. The treatment resulted in more tumour-infiltrating T cells than ACT alone. They also demonstrated that this required the IL-10 receptor and antigen stimulation, confirming that the improvement results from IL-10 recognition by tumour-antigen-specific T cells rather than another process.
Next, they showed that the increase was mainly due to the direct proliferation of terminally exhausted T cells and not the conversion of a different group of T cells, progenitor exhausted T cells, which are still able to proliferate. Furthermore, through experiments where they could sort or deplete progenitor exhausted T cells, they showed that the engineered IL-10 acts directly on terminally exhausted T cells to enhance their proliferation through a process independent of progenitor exhausted T cells.
Further experiments showed that IL-10 enhances metabolism in terminally exhausted T cells by promoting a specific type of oxidative phosphorylation, and the team identified some of the genes and pathways affected by IL-10 treatment.
Finally, the researchers tested the efficacy of IL-10 together with ACT or an immune checkpoint blockade in a variety of mouse cancer models. The treatment induced tumour regression and durable cures, eradicating the majority of established solid tumours. Following the treatments, survivors were very likely to reject tumour cells when they were challenged anew, indicating that they had acquired long-term anti-tumour immune memory. Together with the fact that IL-10 generally has a good safety profile, this suggests that these findings will translate well into clinical treatments.
“We have shown that this combination is effective in preclinical models,” says the study’s lead author, Yugang Guo of the École Polytechnique Fédérale de Lausanne. “In theory, these findings could be incorporated directly into most existing immunotherapies, but of course every new combination must first be tested in clinical trials.”
doi:10.1038/nmiddleeast.2021.50
Guo, Y. et al. Metabolic reprogramming of terminally exhausted CD8+ T cells by IL-10 enhances anti-tumor immunity. Nature Immunology http://dx.doi.org/10.1038/s41590-021-00940-2 (2021).
Stay connected: